Mastitis: what are the symptoms of mastitis and how to treat it
The condition is more common during the first three months of breastfeeding


Parenting advice, hot topics, best buys and family finance tips delivered straight to your inbox.
You are now subscribed
Your newsletter sign-up was successful
The thought of getting mastitis can cause mums unnecessary worry and yet it can be avoided and quite quickly dealt with if it does occur.
Mastitis is a condition that, regardless of breastfeeding positions, can affect many mums who breastfeed their babies, and it can also affect those who decide not to breastfeed. It's a condition that can cause overall breastfeeding pain. And parenting consultant Rachel Fitz-Desorgher, mother-of-four with a 30-year-long career as a specialist midwife and infant feeding consultant, shares her expert take on how to spot the signs and relieve pain. So here is your quick guide to avoiding, spotting and treating mastitis…
What is mastitis?
Mastitis is an inflammation of the breast and is almost always caused by engorgement. Occasionally it is caused by bacteria getting in through a damaged nipple. When breasts get full of milk and, for whatever reason, your baby leaves a lot behind after feeding, you may get a bit of a gridlock of swollen blood vessels and milk.
This can cause tissue fluid to leak, creating even more gridlock. This engorgement leads to inflammation. Although most people assume you have to be a breastfeeding mum to get mastitis, this isn’t true.
Almost all new mums get engorged around day three when the milk “comes in”. So even a mum who has never breastfed can get the inflamed breasts that signal mastitis. Also, nipple piercings and cracked skin can open the way to bacteria getting in and causing infective mastitis.
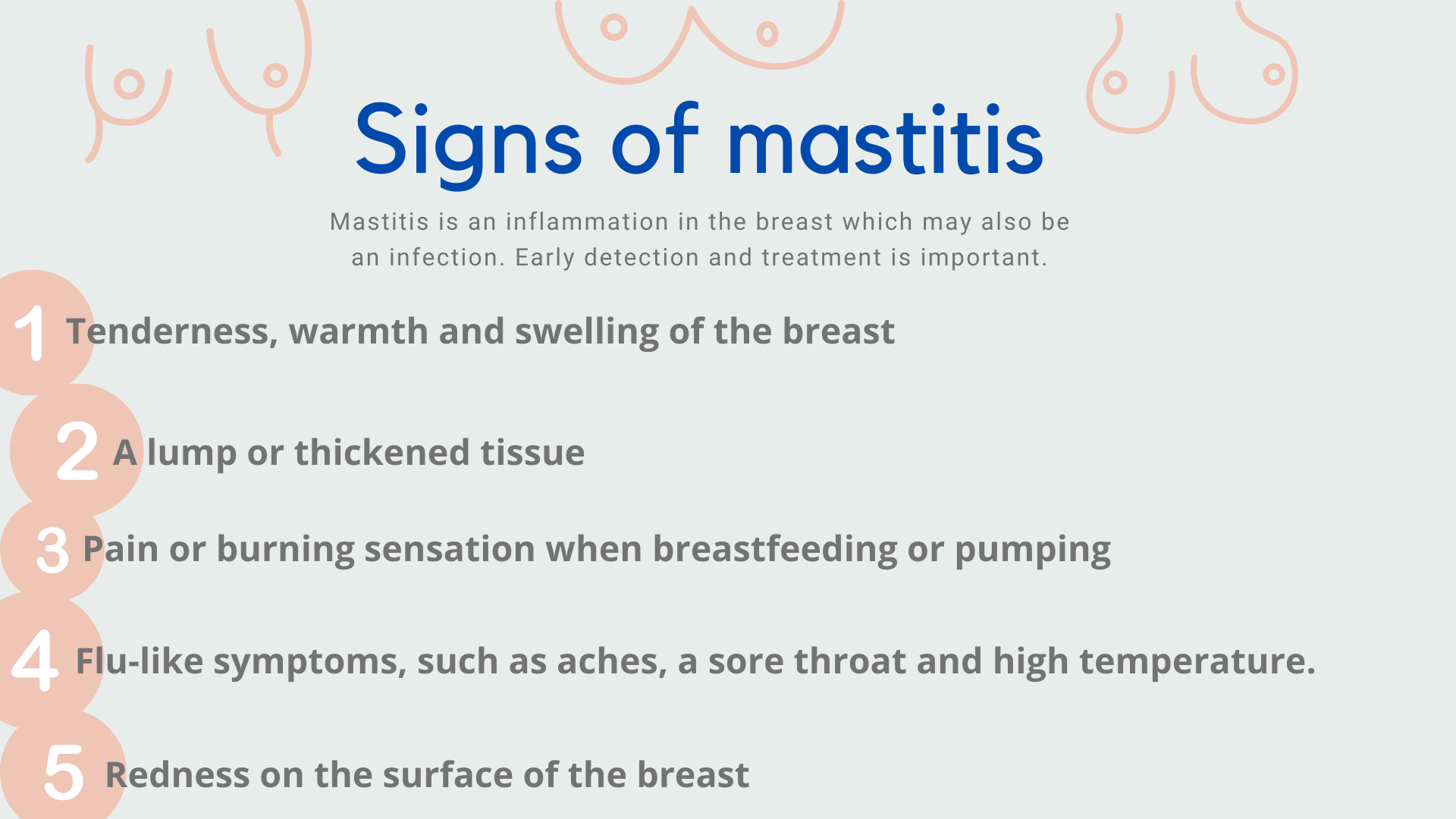
What are the symptoms of mastitis?
People who have mastitis may feel ill. They feel run down or achy. The most common symptoms of mastitis are one or both breasts being red, swollen and hot. A painful lump on the breast and flu-like symptoms, such as aches, a sore throat and high temperature.
Mastitis usually affects only one breast at a time. The symptoms often come on suddenly. But, if you are checking your breasts regularly and gently before feeds, you will spot signs. Other symptoms may include:
Parenting advice, hot topics, best buys and family finance tips delivered straight to your inbox.
- Tenderness, warmth and swelling of the breast
- A lump or thickened tissue
- Pain or burning sensation when breastfeeding or pumping
- Flu like symptoms, such as aches, a sore throat and high temperature
- Redness on surface of breast
What is the treatment for mastitis?
Treatment is in the form of taking regular paracetamol and ibuprofen to reduce pain and inflammation, and to reduce your temperature if it has risen. If you feel poorly, go to bed and drink plenty of fluids. Start this as soon as symptoms appear.
Don’t express but do start doing reverse pressure softening before every feed. Using a flat hand on your breast, firmly massage from the nipple back towards the ribcage. Go all around the breast massaging backwards firmly. This will reduce the engorgement and ease the swelling and tenderness without stimulating more milk to be made. Once you have softened the breast a little, feed your baby.
Let your baby feed for as long (or as little) as they want on one side and then, after a short break and a nappy change, offer the second side for as long as they want.
It is important to let baby lead and not try to interfere in any way by tickling them to make them feed more or taking them off before they are ready. Your baby knows what they are doing and interfering can simply confuse your body, which is trying to work out your baby’s unique needs. Because most mastitis is caused by engorgement and not bacteria, antibiotics should not usually be needed if you treat the problem fast.
Engorgement mastitis is actually self-limiting. If baby leaves a lot of milk behind after feeding then that milk starts to be reabsorbed back into your body. This has the effect of turning down the supply, thereby reversing the mastitis.
This is why expressing to relieve mastitis can make matters worse. The body can’t work out the true needs of your baby and so continues to oversupply. If, despite your efforts, the symptoms persist, you should see your GP. Just occasionally there is a bacterial infection rather than simple inflammation from engorgement and antibiotics are needed.
Can you still breastfeed if you’re suffering with mastitis?
Yes. Although mastitis is painful and can make you feel poorly, it is helpful in your recovery to carry on breastfeeding if you can. Your body needs to know your baby’s needs and the quicker it can work this out, the sooner the mastitis will pass. Try laying down to feed as this can be more comfortable and can also give you a chance to rest.
If you simply cannot get baby onto your breast to feed, express for 20 minutes from each breast which has not been fed off and feed this milk to your baby. Sometimes the milk will have blood in it and, although this looks grim, it will not harm your baby.
How can mastitis be avoided?
You can avoid mastitis by offering your baby both breasts each time and being baby led; in sync with your baby’s natural feeding pattern. It’s best to offer both breasts if you can, at every feed - baby won’t always take both but do offer. Give your little one a nice break of 10-15 minutes between sides and use this time to make yourself a drink and change their nappy.
Common mistakes that can increase the likelihood of engorgement and, therefore, mastitis are;
- Only offering one breast each time
- tickling baby’s chin to keep them continually sucking
- repeatedly putting baby back to the same breast to help them “get more hind milk”
Unless there is a clinical need - like a poorly baby or a poorly mum - try to avoid expressing milk before your baby is 6 weeks old. Expressing sooner than this can confuse your body while it is still trying to work out the unique needs of your little one and this can lead to oversupply, engorgement and mastitis.
Every day, practice good breast care as part of your daily routine;
- examine your breasts carefully for tender spots and lumps.
- Work backwards from the nipple and areola and check the entire breast.
- Any lumps need firm but gentle massage and reverse pressure softening (see above).
This daily care can help to prevent blocked ducts, mastitis and “blebs". Blebs are milk blisters, they usually look like a tiny white or yellow spot about the size of a pin-head on your nipple. The skin surrounding a milk bleb may be red and inflamed, and you may feel pain while breastfeeding.
Although common, mastitis is not an inevitable part of the breastfeeding experience. It’s an exhausting time, but try to look after yourself as best you can. If you can check and massage your breasts daily, feed your baby responsively and on demand you may be lucky enough to avoid suffering from this complaint.
Video of the Week:

Rachel Fitz-Desorgher is a leading, internationally-known baby expert, and parenting mentor. Having worked for over 30 years as a midwife, infant feeding specialist, active birth teacher and parenting consultant, she published her first book, Your Baby Skin To Skin in 2017 and it quickly gathered five-star status with its reviewers. Rachel Fitz-Desorgher has has been featured in several articles for publications including The Daily Mail, The Independent, The Express and Yahoo Lifestyle. She's also a regular contributor for Mother&Baby. When not writing, Rachel runs workshops and presentations on how evolution impacts on baby and parent behaviour, and mentors executive women transitioning from the corporate life to motherhood.