Female contraception: which type is best for me?
Lots of men wear the wrong-size condom according to a new study - and our research shows that 1 in 5 of you aren't using any contraception at all! Our guide will help you decide what's best for you


Parenting advice, hot topics, best buys and family finance tips delivered straight to your inbox.
You are now subscribed
Your newsletter sign-up was successful
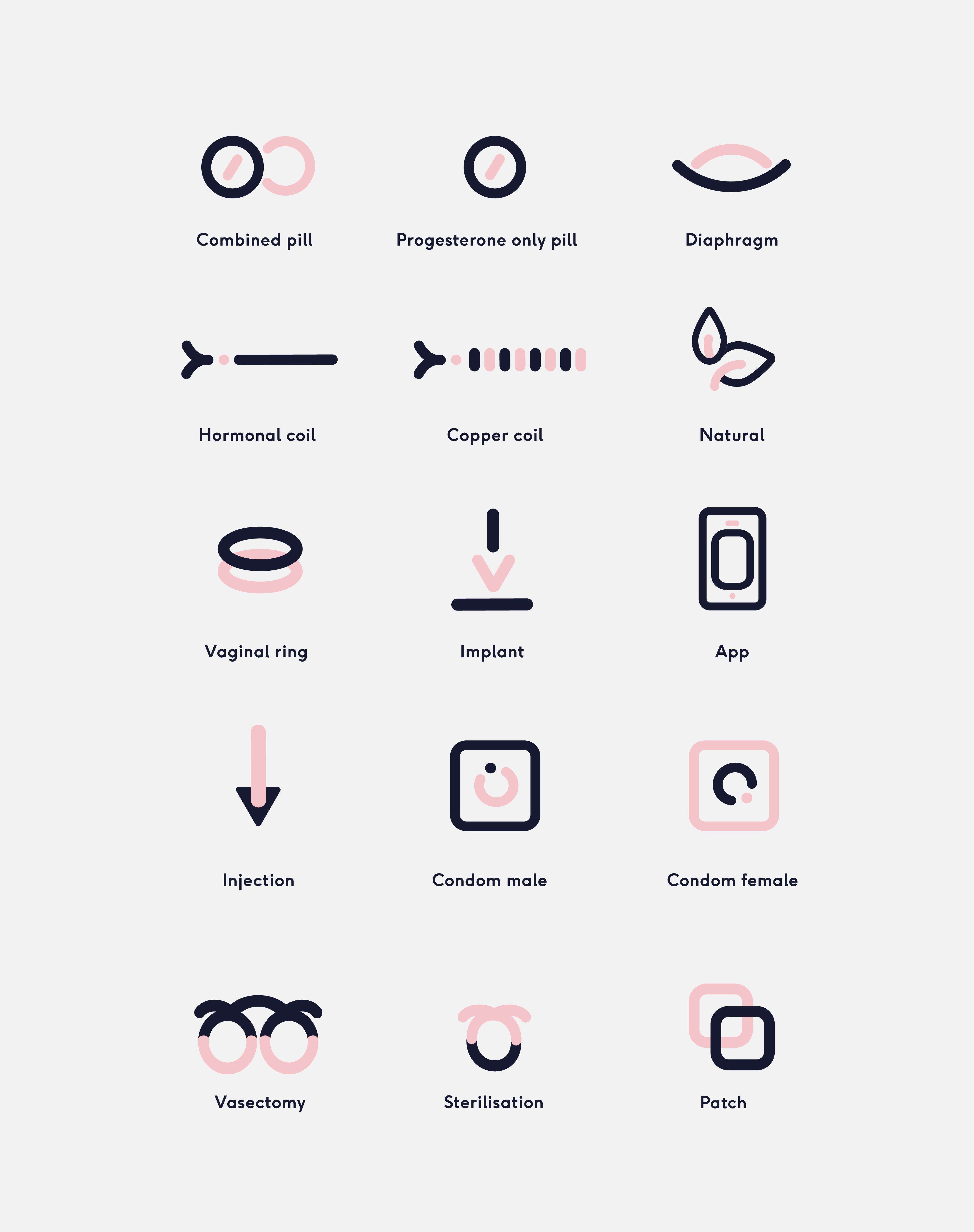
We discuss the pros and cons of popular contraceptive methods – so you can work out which is right for you.
Female contraception - it's a topic that’s getting more and more airtime. The latest female contraception story to hit headlines revolves around the contraceptive patch, after ITV’s Love Island’s Rebecca Gormley was spotted wearing this method of contraceptive in the villa. The reality star has been praised for her sex-positive message, with one fan declaring on twitter, ‘there is zero shame in looking after your sexual health’.
The contraceptive patch is a transdermal patch applied to the skin that releases synthetic oestrogen and progestogen hormones to prevent pregnancy and was first available to women in 2002; it's just one of the new female contraception options out there. But despite complaints of moods swings, weight gain and even depression, the pill is still by far the most popular choice, with nine out of 10 women using female contraception opting for it.
Research conducted by Superdrug showed that 30% of women spend less than 30 mins researching their contraceptive options, while 85% spend more than 30 mins getting ready for a night out. Enter The Lowdown, hailed as the 'Trip Advisor for female contraception'.
The Lowdown provides women with an online space to share their experiences of contraception, offering real, honest reviews that will help others decide which contraceptive is right for them.
"Using something that doesn't suit you and your body can really impact your life and mental health. And if you're not satisfied with your contraception it makes you more likely to stop using properly, making it less effective," founder Alice Pelton told GoodtoKnow. "I set up The Lowdown because I realised that I couldn't find user based data on real women’s experiences and side effects from contraception anywhere.
"It's not an easy choice to make - our findings show that almost half of women had trouble trying to find a method of contraception that suited them, and 78% of women have experienced unwanted side effects from their contraception. But it's worth persevering; for many of us contraception is an absolute necessity and something that we use for decades. Also what's 'right' for a woman isn't static - our bodies, hormones, needs and lifestyles change, and our contraception often needs to change too."
Parenting advice, hot topics, best buys and family finance tips delivered straight to your inbox.
You can leave a review on The Lowdown here.
So which method of female contraception is right for you?
The contraceptive patch
Also known as: Evra
How does it work?
The patch releases a daily dose of hormones through the skin into the bloodstream - the same hormones as the combined pill (oestrogen and progestogen). This works in the same way as the pill, by preventing the release of an egg each month (ovulation).
The contraceptive patch also thickens cervical mucus, making it more difficult for sperm to progress, and thins the womb lining so a fertilised egg is less likely to be able to implant itself.
How do you take it?
The patch needs to be applied to clean, dry skin and changed once a week. You change the patch every week for three weeks, and then have a week off.
How effective is it?
Used properly, it's 99% effective. It won't work as well if the skin the contraceptive patch is applied to is hairy or damp.
What are the good points about it?
Unlike with the pill, you don't need to think about it every day and it's still effective if you're sick, or have diarrhoea. You can even wear the patch when you're playing sports, swimming or in the bath.
What are the bad points about it?
The patch can raise your blood pressure, and some women get temporary side effects, such as headaches. Rarely, some women may develop a blood clot when using the patch.
You need to use condoms during sex when wearing the contraceptive patch to protect from STIs.
Combined Pill
There are two types of pill: the combined pill, which contains the hormones oestrogen and progestogen, and the progestogen-only pill.
Also known as: the 'ordinary pill'
How does it work?
The hormones in it stop you from releasing an egg each month so it can't be fertilised. It also makes your cervix (the opening at the neck of the womb) thicker so it's harder for sperm to get through, and makes your womb lining thinner so it can't support any fertilised eggs.
How do you take it?
You take one tablet every day for 21 days. Previously, it was thought you would have to take a seven-day break before you start a new pack, but recent FRSH guidelines suggest the seven-day break may be pretty pointless. You can take a break, or continue taking packs back to back.
How effective is it?
If taken properly, it's 99.8% effective. Although sickness, diarrhoea and taking antibiotics can all make it less effective or stop it from working completely. If you're worried, use condoms as well. Using condoms will also protect you from sexually transmitted infections.
What are the good points about it?
It can stop period pain, and make periods shorter and lighter. It can also be used to help with acne. This is why some teenagers are prescribed the pill, even if they're not having sex yet.
What are the bad points about it?
Some side effects include headaches, nausea, weight gain, tender breasts and occasionally some small spots of blood, between periods. These effects usually go away after the first few packs but if they don't, speak to your doctor because there are 22 different brands of combined pill. It also doesn't protect you from sexually transmitted infections.
You need to use condoms during sex for this. Taking the pill does give you a slight increased risk of blood clots, but you'll need to pass a health check before it is prescribed to make sure you're not at high risk of this.
Progestogen-only Pill
Also known as: 'POP' or the 'mini-pill'
How does it work?
It thickens the cervix so it's harder for sperm to get through, it makes the womb lining thinner and some of them, such as Cerazette, stop you ovulating (or producing an egg).
How do you take it?
You take one tablet every day for 28 days. You don't have a break with the mini-pill and it's important you take it at the same time every day. Taking it even three hours late can increase the chance of getting pregnant. Use condoms to be on the safe side if this happens. Condoms can protect you against sexually transmitted infections too.
How effective is it?
It's not as effective as the combined pill but is 90-99% safe. Being overweight can make it less effective too. Speak to your doctor if you're worried.
What are the good points about it?
It gives you fewer problems than the combined pill and is especially good for breastfeeding mums (the combined pill can stop milk being produced), women who can't take oestrogen, women at risk of heart disease or strokes and heavy smokers.
What are the bad points about it?
Some side effects include irregular periods, or your periods could stop completely, spots, nausea and headaches. If you've had an ectopic pregnancy, breast cancer or abnormally high cholesterol your doctor might not give it to you. As with the combined pill, the progestogen-only pill does give you a slight increased risk of blood clots, but you'll need to pass a health check before it is prescribed to make sure you're not at high risk of this.
Female condoms
Also known as: Femidom
How do I use it and how does it work?
How to put it in is described inside the packet, with diagrams. It has a ring on the end of it which holds it in place and, if inserted properly, stops the sperm getting into the womb. Always take care when taking it out the packet because rings and long fingernails could rip it. Also take care when you take it out after sex to avoid spillages. It can then just be thrown away. Don't flush it down the loo and don't re-use it.
How effective is it?
If put on and used properly it is 99.9% effective. If it slips or splits, speak to your doctor or family planning clinic straight away.
What are the good points about it?
There are no major side effects of using one and if put on properly, it's completely effective. It can also protect from sexually-transmitted diseases. Femidoms aren't made of latex so this reduces the chance of an allergic reaction, and being damaged by oil-based lubricants.
What are the bad points about it?
Putting them in can be difficult the first time and, because of this, they aren't as popular as male condoms.
The injection
Also known as: Depo
Where can I get it and how does it work?
The contraceptive progestogen is injected at 8 or 12 week intervals at your family planning clinic and some doctor's surgeries. This hormone thickens the cervix so it's harder for sperm to get through, it makes the womb lining thinner and it stops an egg being produced.
How effective is it?
It's 99% effective.
What are the good points about it?
If you don't like taking pills, then injections are a good idea and you can get them for free from your family planning clinic. It lasts for the full 8 or 12 weeks. Both of the jabs have also been found to help protect against ovarian cysts and ectopic pregnancies.
What are the bad points about it?
You have to go back to the clinic to have it every 8 or 12 weeks. It can cause heavy, irregular or longer periods and some women stop having periods altogether. You can get headaches and experience weight gain and it can take you, on average, up to 18 months to be fully fertile again after you stop having it. They also don't protect you from sexually transmitted infections. You will need to use condoms during sex for this.
The implant
The implant is a small, bendy tube that is put under the skin in your upper arm. In the UK the only one available, currently, is called Implanon.
Where can I get it?
The implant is inserted into your arm using an injection. This is usually done by your GP but some family planning clinics can do it too. You're given a local anaesthetic and putting it in is quick and painless, although you could get a slight bruise from the injection. You can feel the implant, but not see it.
How does it work?
It lasts for up to three years, although it can be taken out sooner if you want. Whereas the injection gives you a high dose of progestogen, which decreases over 8-12 weeks, the implant releases a steady stream of the hormone into your blood every day. This thickens the cervix so it's harder for sperm to get through, makes the womb lining thinner and stops an egg being produced.
How effective is it?
It's over 99% effective. Being obese can stop it from being as effective, so speak to your doctor if you're worried.
What are the good points about it?
Once it's in, that's it for three years. No worrying about booking repeat appointments or taking pills. Your normal level of fertility returns straight away, after it's removed. You can breastfeed with the implant in too.
What are the bad points about it?
They can cause headaches, acne and weight gain and your periods are likely to change. You might even notice a change in sex drive too. Your doctor or clinic will need to order the implants in so you'll need to talk to them, in advance, if you want one. The doctor will also need to remove it too. They don't protect you from sexually transmitted infections. You will need to use condoms during sex for this.
The coil
It's very small - not much longer than a matchstick, and is T-shaped. It's normally made of plastic and copper. Your womb (uterus) is actually only about the size of your clenched fist so if you put a matchstick in your palm that will show you how it fits.
Also known as: Intrauterine device, IUD
Where can I get it?
Some trained GPs and nurses can insert it, but it's most commonly available through your family planning clinic. Gynaecologists can fit them too. IUDs fold up and are then pushed through your vagina and expand into your womb. All coils have either one or two little threads, which hang down into your vagina. The doctor or nurse will use these to check that it's in place. They will also use them to remove it.
How does it work?
The coil stops your partner's sperm from getting into your womb. It changes the thickness of your cervix and makes it difficult for an egg to settle in the womb lining. It can also last from between 5-8 years depending on the make.
How effective is it?
It's 98% effective.
What are the good points about it?
Once it's in, that's it for 5-8 years. No worrying about booking repeat appointments or taking pills. Your normal level of fertility returns quickly after it's removed. Although some women find it painful when it's inserted and taken out, this is quite rare.
What are the bad points about it?
They can make your periods heavier, longer and sometimes more painful. Your doctor or clinic will need to order the coil in so you'll need to talk to them in advance if you want one. They don't protect you from sexually transmitted infections. You will need to use condoms during sex for this.
The morning after pill
If you've had a mishap with your contraception - or you had unprotected sex, you don't necessarily need to panic. You can buy the morning after pill, Levonelle, over the counter - and it's effective up to 3 days after you had sex. You can also get EllaOne - which is effective up to 5 days after having sex - on prescription.
Levonelle
Also known as: Levonorgestrel
How does it work?
It uses hormones to prevent or delay ovulation and prevent an egg from implanting in the womb.
How do you take it?
It is taken orally and can be used up to 72 hours (3 days) after sex. However, it is more effective the sooner you take it. You can buy Levonelle over the counter (as long as you are over 16) or get it for free on prescription.
How effective is it?
If it's taken within 24 hours of having unprotected sex, it is effective about 95% of the time. Between 25 - 48 hours it is 85% effective and between 49 and 72 hours it is 58% effective.
What are the good points about it?
If your contraception fails or you forgot to use any, you can take this. Side effects are uncommon.
What are the bad points about it?
It's not as reliable as planned contraception, so shouldn't be used regularly as contraception.
EllaOne
Also known as: Ulipristal acetate
How does it work?
As with Levonelle, it uses hormones to prevent or delay ovulation and to stop an egg from implanting in the womb.
How do you take it?
It is also taken orally and can be used up to 120 hours (5 days) after having unprotected sex. You can only get EllaOne on prescription.
How effective is it?
Trials show it is as effective as Levonelle when taken within 3 days of having unprotected sex. New studies are needed to show exactly how effective it is after 3 days.
What are the good points about it?
Again, side effects are uncommon - and you can fall back on it if regular contraception fails.
What are the bad points about it?
As you need a prescription to get it, it could be more difficult to get hold of than Levonelle. And it's not as reliable as planned contraception, so should only be used in emergencies.
Visit your local family planning clinic
Family planning clinics offer free, confidential advice and information on the best contraception to use, how to go about getting it, as well as advice on sexual health and pregnancy. You can also have STI checks.
Anyone can use a family planning clinic, even under 16s, and you can either just turn up for an appointment or get referred there by your doctor. Some clinics offer 'open surgeries' where you can turn up, take a number and wait in line. For more specific information, or for fitting implants and coils, you might need to make an appointment to see a doctor.
The first time you go, you will have to give some contact details and the details of your doctor. They will normally take your blood pressure, weigh you, measure your height and ask you some questions about your health.
Although clinics do differ, the majority provide the following services:
- advice about contraception, including vasectomy and hysterectomy - the combined pill the mini-pill
- contraceptive injections
- free condoms
- free emergency contraception - smear tests/cervical screening, - free pregnancy tests, fertility advice
- fitting and checking of implants and coils (intrauterine devices or IUDs). Some clinics can remove them as well.
- Some of them may also offer advice about rape and sexual abuse, abortion and the menopause and can refer you for counselling if necessary.
You can get details of your nearest family planning clinic from your phone book, doctor, hospital or from the Family Planning Association (FPA).
What new contraception methods are coming in 2020?
We asked Alice Pelton, of The Lowdown, for her thoughts.
"I'm quite excited by a new type of non-hormonal IUD that is currently being rolled out (from Jan 2020) on the NHS, called the Ballerine. It's called an Intrauterine Ball, and is made of a a string of alloy called Nitinol that covered in copper balls.
"When it’s inserted into the womb via a tube, this special shape memory alloy automatically rebuilds itself into a round and smooth ball shape . This round shape is said to reduce the risk of complications, and some early studies have shown it made reduce some of the bleeding and pain that comes with the T-shaped Copper IUD."
Talk any method of contraception through with a health care professional, to find out if it's right for you.
Lauren is a senior content editor covering everything from the latest royal news to fashion, beauty and health content. Lauren graduated from her masters in magazine journalism in 2011, quickly making the transition over to digital and has never looked back. From getting out a breaking news story to penning an in-depth feature, she loves the variety of writing for digital platforms.
