Infertility: Common causes, fertility treatments, IVF and more
If you're having trouble getting pregnant, you could be feeling very upset and isolated, but up to 15 to 20 per cent of people may experience this problem.


Fertility expert Dr Larisa discusses the common causes of infertility and the wide range of treatments available to couples struggling to conceive.
Infertility is medically defined as the inability to become pregnant after 12 months of regular sexual intercourse without birth control or, for women over age 35, six months. Up to 15 to 20 per cent of people may experience this problem over their lifetime, with 1 in 6 couples being affected.
What causes infertility?
For pregnancy to be successful, a sequence of events needs to occur that includes a healthy egg meeting a healthy sperm to create an embryo, that must divide and implant correctly in the womb. It sounds simple enough, yet each one of these processes depends on many other factors and favourable conditions which allow for conception to take place. There may be problems at any of these stages in both men and women.
What can cause infertility in a woman?
Up to 50 per cent of infertility cases happen because of problems with the woman’s fertility and there are many different reasons for this – here are a few of the main ones:
Age: This is the most important factor affecting a woman’s fertility. Older women are less fertile. The chance of a woman conceiving after aged 35 – 39 is about half of women aged 19 – 26.
Even before menopause, our bodies’ reproductive capabilities slow down. This natural decline of fertility happens in all women, though it happens at different ages for individual women. It leads to a reduction in the number of eggs, their quality and therefore ability to fertilise and lead to a healthy embryo. This decline can sometimes be due to previous surgery, cancer treatment or genetic factors.
Ovulation problems: Problems with ovulation are also very common, the biggest cause being polycystic ovaries (PCOS). This a a hormonal and metabolic disorder that leads to irregular ovulation as well as problems with insulin, putting a woman at risk of other health issues too. Ovulation problems may also be due to thyroid disorders, adrenal gland disorders, excessive exercise, diabetes, weight loss, obesity, or certain medications.
Parenting advice, hot topics, best buys and family finance tips delivered straight to your inbox.
Implanting problems: Sometimes the cause is structural problems, or blocked fallopian tubes that transport the sperm to the egg. This can be due to endometriosis, pelvic inflammatory disease (PID), or scarring due to surgery or repeated injury. Sometimes women are born with abnormalities that affect their reproductive organs, and other times fibroids, which are benign growths of muscular tissue in the womb, can create a problem, though not always and it depends on their size and position.
Endometriosis in particular, is a very common condition that causes 1 in 20 cases of infertility. It’s where tissue from the lining of the uterus is found outside the uterus in the pelvis. As well as causing scarring, it can also cause painful and heavy periods, as well as having an effect on your fertility, but it can be a difficult condition to recognise, with diagnosis sometimes requiring several years.

What can cause infertility in males?
Around 30 per cent of infertility cases happen because of a problem with male fertility.
Sperm disorders: Men are also affected by infertility and the issues arise either due to problems producing or having enough sperm, how well the sperm are moving, and whether they are morphologically normal or not. Whereas a woman is born with all the eggs she will ever have in her lifetime, a man produces new sperm every 3 months, but men are still not immune to the effects of age and over the age of about 40, sperm quality declines.
Genetic conditions: Men can be born with genetic conditions, such as cystic fibrosis, that can prevent them from producing sperm in an ejaculate, but more commonly, there could be structural problems such as varicoceles, which are enlarged veins affecting a man’s testicles, blocked or damaged reproductive structures that transport sperm, problems with erection or ejaculation, and also previous undescended or injured testicles.
Lifestyle: A low sperm count can be caused by a number of factors from illness and side effects of medication to diet. Environmental and lifestyle factors can affect sperm count too, e.g. too much heat to the testes can lower sperm count as can exposure to certain chemicals. Alcohol and drug misuse and some sexually transmitted diseases can also affect sperm count.
Unexplained infertility
This is perhaps the most frustrating diagnosis of all and affects about a third of couples. No obvious cause for infertility is found despite investigations. But this is where perhaps lifestyle factors may have the most significant influence.
Whereas medical intervention here in the form of IVF is often given, it may not necessarily succeed, with success rates still lower than we would hope to see. This is why identifying any potential causes behind the infertility is really important, including any lifestyle factors that need to be adjusted before treatment is started.
Treating infertility: How can you get pregnant if you are infertile?
See your GP if you're concerned and have been trying naturally between 6 months to a year, depending on your age. It’s important to investigate the infertility first, for both you and your partner. Tests can be as simple as a blood test to check your hormone levels and a pelvic ultrasound to look at the ovaries and womb. A semen sample from your partner can be checked for sperm levels.
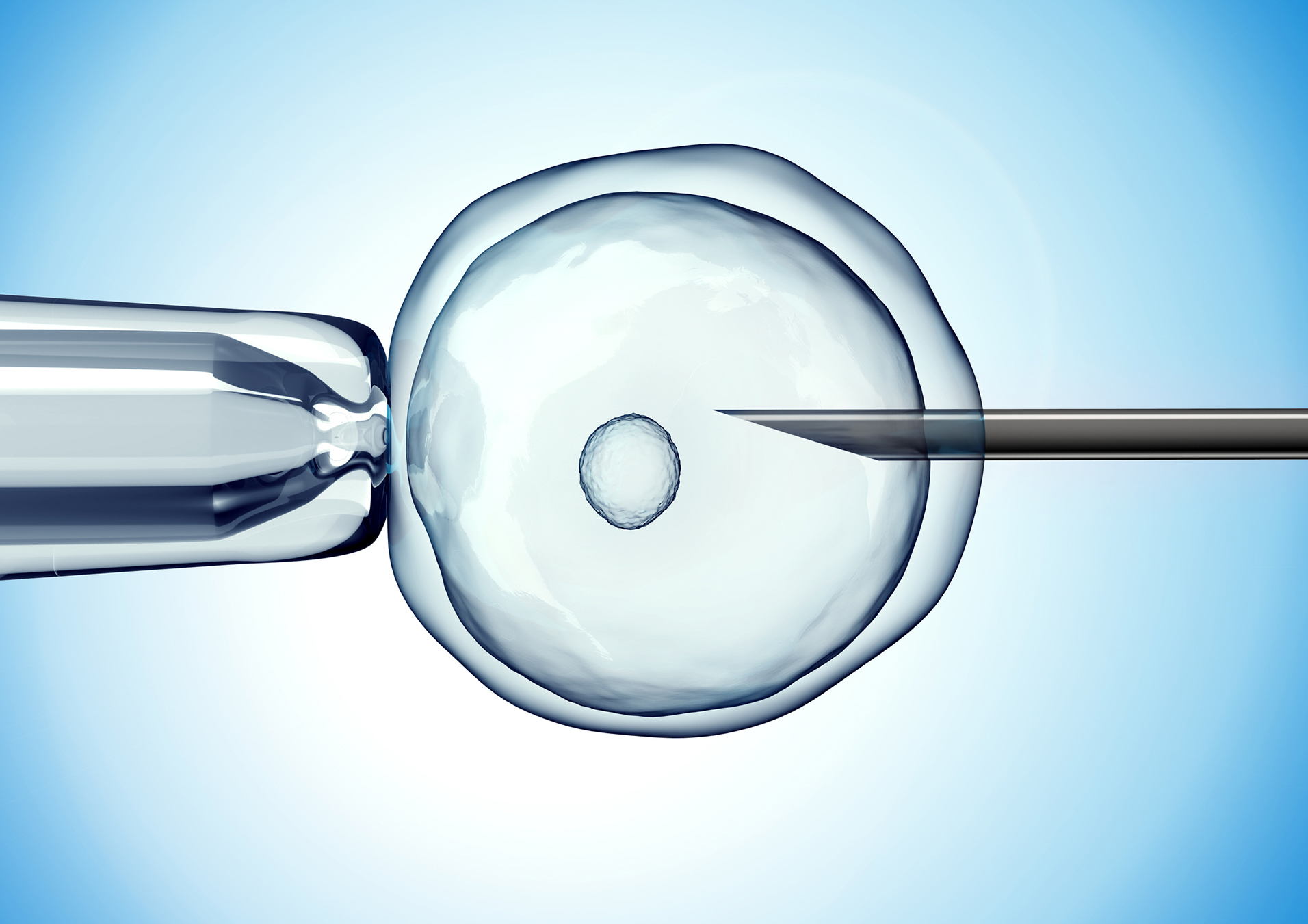
Other treatments, from donor sperm, to assisted conception techniques such as in vitro fertilisation (IVF) or intracytoplasmic sperm injection (ICSI), where a single sperm is injected into an egg and then the embryo is placed back in the womb, can be discussed with you.
But before any of this starts, it’s vital to get yourself into the best possible state of health through lifestyle changes that will improve any underlying medical conditions that could be behind the infertility, as well as boosting your chances of pregnancy whether naturally or through assisted reproductive treatment.
This is the foundation of The Conception Plan, which I use to improve a couple’s natural chances of conception, as well as those undergoing treatment, and I discuss these tips in my article on how to get pregnant.
IVF
Around 24,000 couples opt for IVF (in vitro fertilization) treatment every year in the UK. About 8000 babies are conceived through IVF procedures, which involve removing eggs from the woman's ovaries and mixing them with either her partner's or a donor's sperm to fertilise. The fertilised eggs are then put back in the womb.
Do keep in mind that NHS treatment availability varies throughout the UK and you may have heard of the postcode lottery.
The funding is severely restricted in many areas of the UK and national guidance is not necessarily followed, instead being replaced by very strict criteria that have to be met for a couple to qualify for treatment. You could need several IVF treatments before you conceive and there's no guarantee then that you will end up with a baby.
IVF treatment can be very gruelling, so aim to get as much help and support from family and friends or support groups as you can. Not everyone will get pregnant with IVF and some of these pregnancies may end in miscarriage. Choose a clinic that is licensed by the Human Fertilisation and Embryology Authority (HFEA), which regulates and inspects all clinics and if you are going abroad, make sure you do your research about the clinic and its success rates.
Infertility treatments overview
Ultimately, treatment is all about reversing an identified cause. There are times when a doctor may recommend surgery prior to undertaking any fertility treatment, if the lifestyle changes alone are not enough to improve the clinical picture.
For example, this can be done for endometriosis, polycystic ovaries, blocked fallopian tubes, scarring in the womb, or for male related infertility due to a previous vasectomy, or problems with ejaculation where sperm needs to be retrieved surgically from the testes.
Fertility treatment typically involves the stimulation of egg or sperm production, or the handling of eggs, sperm or embryos. It can include treatment with clomid, intrauterine insemination (IUI), in vitro fertilisation (IVF) or intracytoplasmic sperm injection (ICSI). It may also involve the use of donor eggs and sperm, as well as surrogacy.
Superovulation drugs
Suitable for: Women with ovulation problems, most commonly PCOS. What happens? Clomid (taken as a pill) or Gonal-f, and Menopur (administered by injection) will be prescribed to encourage the ovaries to produce more eggs than usual. Side effects: Hot flushes, mood swings, nausea and ovarian hyperstimulation syndrome (OHSS), a rare but potentially life compromising condition. There is a higher chance of twins. Private cost: Clomid costs less than £10 for a prescription; the injectable drugs are around £200 per cycle, but you will need monitoring by ultrasound and blood tests.
Intrauterine insemination (IUI)
Suitable for: Women for whom superovulation hasn't worked; mild male factor infertility; if using donor sperm, in cases where a couple is unable to have sex. What happens? You take superovulatory drugs (though you could have IUI naturally without this) and have ultrasound scans to track the development of your eggs. Once your eggs are mature, you will be given a shot of the hormone HCG to trigger ovulation and the IUI is done after this. Your partner produces a semen sample or donor sperm is used and inseminated into the uterus - this takes about 10 minutes and is pretty painless. Before doing IUI, it’s important to make sure a woman’s fallopian tubes are open and healthy. Side effects: Mild cramps, OHSS if stimulating drugs are used, which also increase the chance of twins. Private cost: £800 to £1300 per cycle
In vitro fertilisation (IVF) and Intracytoplasmic sperm injection ICSI
Suitable for: Women for whom superovulation and IUI has failed, unexplained infertility, endometriosis, absence of fallopian tubes or pelvic inflammatory disease, older women, male factor infertility. What happens? Fertility drugs are used to stimulate the ovaries to produce eggs. Assuming all goes well at this stage, those eggs are then retrieved from the woman's ovaries in an out-patient procedure, and fertilised in a special incubating dish with sperm or, in cases of ICSI, sperm is injected directly into the egg to help with the process of fertilisation. Side effects: Hot flushes, headaches, bloating, OHSS, small surgical risk with egg collection process. Private cost: This can be anywhere from around £5000 per cycle, to much more, also depending on whether any add ons are used. You doctor should always discuss these with you, as the majority of these have not yet got a robust enough evidence basis behind them.

Donor eggs
Suitable for: Older women, those with premature menopause or very low ovarian reserve of eggs, where several rounds of IVF has failed, same sex male couples using a surrogate, you have a high risk of passing on an inherited condition. What happens? A younger woman who has been screened by the clinic undergoes treatment with fertility drugs in order to collect her eggs, which are then fertilised with sperm from your partner to create an embryo that is transferred into your uterus. In the meantime, you will take medication to prepare your womb lining ready to receive the embryo. Private cost: Depending on the criteria you may have for the donor, this can be anywhere from £10000 upwards, with fresh eggs costing more than those that have been frozen.
Donor sperm
Suitable for: Women who are single, male factor infertility, same sex female couples, there is a high risk of the male partner passing on an inherited condition. What happens: Donor sperm can be used either in the process of IUI or IVF. Side effects: The sperm should come from a regulated clinic to ensure that it has been screened appropriately. Unregulated sperm donation done online puts the woman’s and her baby’s health at risk. Private cost: Costs normally start at around £1000.
Surrogacy
Suitable for: Women who do not have a uterus or have problems affecting the uterus, cases where repeat IVF has failed, same sex male couples using an egg donor. What happens? A surrogate is a woman who undergoes embryo transfer and carries the pregnancy. Private cost: There is no set figure on this and costs can be huge depending on where the surrogacy is done. However, an average cost of £12000 to £15000 is common in the UK. Surrogacy laws are different in each country, and can be quite complex.
Dr Larisa Corda is an obstetrician and gynaecologist and one of the UK’s leading fertility specialists

Dr Larisa Corda is an obstetrician and gynaecologist and one of the UK’s leading fertility specialists. She qualified from Imperial College London with her training taking place in both the UK and Australia. This has seen her gain an understanding and appreciation of gynaecological, obstetric and fertility issues across a wide international population. Larisa believes in a holistic approach to treating a patient that addresses many lifestyle factors as well as a combination of Eastern and Western medical approaches. Larisa is ITV This Morning’s and Channel Mum’s Fertility Expert, where she can regularly be seen on screen sharing her expert advice.